|
A life without worry is a dangerous thing. It would mean a lack of concern for consequences of our actions, a reduction in reflective thinking and a reduced drive to get things done by a deadline. It would mean we would step out in front of the busy road, or test if the iron is hot by using our finger. Worry has been a safety mechanism for us throughout the evolutionary process, and has help ensure our survival. The point being, that a little bit of worry is a good thing. The other end of the scale is a debilitating experience when we cannot think of anything but mistakes we have made or have a fear of the future that is enough to make us physically sick and interrupt our lives. So how do we know when to worry about worry? How much is enough? And how to help foster a sense of safety without taking away our children’s ability to experience worry and instead learn to cope with it? If compared to other children you see that your child gets worried more often, and more intensely than others, and things have persisted for some time, then it might be time to get some professional support. Other signs to look out for include irritability, avoidance of things they might have previously enjoyed, physical complaints like a sore tummy, or comments like things being ‘boring’ or ‘stupid’, when they may in fact be difficult and your child is feeling afraid. Not wanting to go to school or see friends can be a red flag for a child experiencing anxiety. As a parent, there are some things you can do at home to help foster a sense of resilience to things that may be worrying and help your child cope with those feelings. Some possible ways include:
The relationship building that you do with your child will ultimately underpin these strategies. Being able to give them the confidence to believe what you say, to confide in you, and to give them the feeling of independence and competence to take on the world. Don’t minimise the positive interactions that you have together in the big jigsaw puzzle of your child’s world. Plant the seeds of the relationship when they are 5, so they know when they are 15, that you are cheering them on. Alyce Galea, Psychologist Emotional intelligence refers to the ability to identify, use, understand and manage emotions in a positive way to relieve stress, communicate effectively, empathise with others, overcome challenges and diffuse conflict.
Emotional intelligence impacts many different aspects of your daily life, such as the way you behave and the way you interact with others. If you have a high emotional intelligence you are able to recognise your own emotional state and the emotional states of others and engage with people in a way that draws them to you. You can use this understanding of emotions to relate better to other people, form healthier relationships, achieve greater success at school, and lead a more fulfilling life. Emotional intelligence consists of four attributes:
Book an appointment with one of our psychologists to learn ways to improve yours or your child's emotional intelligence As complex and daunting as aggressive behaviour can appear, the way to respond can be simple and involves answering 3 questions:
1. What emotions am I (as the parent or carer) feeling right now? If we are not emotionally regulated when we respond to a child, there is a high likelihood that this will only perpetuate the situation. The child’s need remains unmet and they now also have additional stress. As the saying goes (and neuroscience attests to), ‘when we are at our angriest… we are at our stupidest’. Speaking of, when children are highly emotionally dysregulated they don’t have access to their pre-frontal cortex which is responsible for problem-solving, reasoning and perspective taking. So, asking them to ‘make a good choice’ at the height of aggressive behaviour probably isn’t going to work. We should try and emulate what we can see a duck in a pond look like; on the surface it is calm and graceful, underneath is a little more frantic but that is hidden from view. 2. How are environmental factors influencing the situation? Many times, behaviours are influenced by those observing it. Removing other children or adults can be the catalyst for de-escalation. Similarly, removing yourself partially or fully as a responder (when safe to do so) can also be what is required for de-escalation to occur. 3. What does my child feel, need or want? Behaviour is almost always a form of communication that expresses a need. Identifying and reflecting back your child’s need or feeling goes halfway to solving the problem. There is a difference between caving into unrealistic demands and simply demonstrating to your child that you can hear and understand their frustration. Children may need up to a few hours to recover and return to a baseline state. This is the time to have that conversation about what they can do to get their needs met next time in a more adaptive way. If you are seeking parenting support or support for your child, please contact the clinic to book an appointment with one of our psychologists. The way we view our bodies has a huge impact on how we feel about ourselves and how we live our lives. Our perception of our bodies and the bodies of others starts to take shape early, and can be influenced greatly by our family’s values and beliefs, but also by ours peers and broader influences like the media. Unfortunately, from a young age children begin to show dissatisfaction and concern about their appearance and weight, which can then lead to engaging in behaviours that attempt to control or change their young bodies. By the end of the teenage years, most young people have been on a diet of some kind. As adults, the majority of women wish to lose weight (even those who are in the healthy weight range!) and approximately two-thirds of women withdraw from activities due to feeling negatively about their bodies. So how can we move towards being more accepting of our bodies and feeling better about ourselves? Here are some tips on how to build a better relationship with your body:
Social Media, Selfies and Self-Esteem: 4 questions to ask your teen and helpful messages to discuss13/5/2024
How can you support your teen’s development in the age of social media? Self-esteem development during adolescence is an important area of focus for psychology. Self-esteem refers to the judgements young people make about their worth as a person and is closely associated with mental well-being. The way that we are communicating with peers has changed dramatically over the past decade with the growth of social media platforms such as Facebook and Instagram. Although social media has made communication and keeping up with peers easier, it has brought about an added pressure to adolescent’s self-esteem development. It has never been easier to compare yourself to peers than it is right now. On social media, your life is on show and young people are able to create a beautiful ‘highlights reel’ which is often unrealistic and highly filtered. This in turn feeds comparison to unachievable standards and can leave you feeling not good enough. Here are some conversation starters to have with your adolescents as well as some helpful messages that we need to be sending about social media. Sit down with your adolescent and ask them: “What does it feel like when your post doesn’t get many likes?” Helpful messages to discuss:
Look at Instafamous celebrities’ profiles with your child and ask, “What do you think about this person’s profile? What does their life look like to you?” Helpful messages to discuss:
“How do you feel when you compare your number of ‘friends’ to other people’s number of ‘friends’?”
"What inspires you on your social media feeds?"
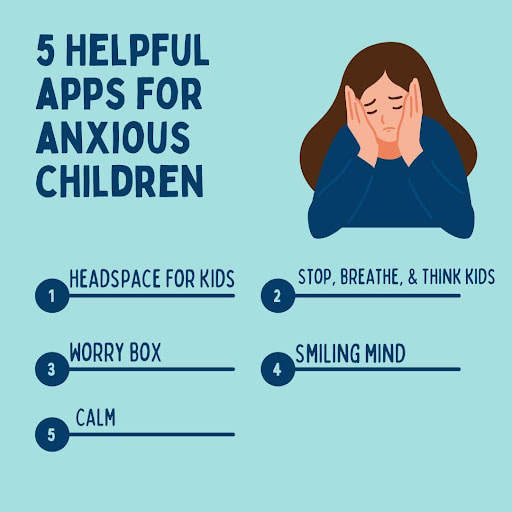
Helping your teens to think about their motivations behind posting up that hundredth sexy selfie will help them (and you) to think about healthier ways of getting validation and building self-esteem. It’s probably not going to drastically change their posting behaviour, but it might help them to see their online behaviour through a new lens. Through having this conversation, you might be able to come up with ideas about other ways to feel confident – such as learning about their strengths and building on them. This is how positive self-esteem is developed. It might even help you to reflect on whether your child has enough opportunities to experience success and develop their strengths. If not, think about how you can facilitate this by increasing their opportunities in the ‘offline’ world. Remember, social media is a big part of your teens life so understanding more about it will help you to show your interest in your child’s life bringing you closer together which is so important for your relationship. If you have concerns about negative impacts that social media is having on your child’s self-esteem and you are unsure how to tackle this, speak with a psychologist skilled in this area. While some level of anxiety is normal in children, excessive anxiety can interfere with a child’s daily activities or quality of life. There are several apps available that can help children manage their anxiety. It can provide children with tools and strategies to help them identify, challenge, and reframe negative thoughts, as well as develop emotional intelligence and mindfulness. Here are 5 helpful apps to help support an anxious child: 1. Headspace for Kids: Headspace is a popular mindfulness app that offers a special section for kids. This app provides a range of guided meditations, breathing exercises, and visualizations that are designed to help children manage their anxiety and stress. 2. Stop, Breathe & Think Kids: This app uses fun and engaging activities to help children develop emotional intelligence and mindfulness. It includes a range of guided meditations, breathing exercises, and mindful activities that can help children manage anxiety and improve their overall well-being. 3. Worry Box: Worry Box is a cognitive-behavioural therapy app designed to help children cope with worry and anxiety. The app offers a range of tools and strategies to help children identify, challenge, and reframe negative thoughts. 4. Smiling Mind: Smiling Mind is a mindfulness app designed specifically for children and adolescents. The app offers guided meditations and mindfulness exercises that are tailored to the age and developmental stage of the user. 5. Calm. This app is a popular meditation and relaxation app that offers a range of guided meditations and breathing exercises that can help children manage anxiety and stress. The app also offers sleep stories and other relaxation techniques that can help children calm down and relax before bed. It is important to note that while these apps can be helpful, they should not be used as a replacement for professional help. If a child’s anxiety is severe or interferes with daily activities, it is important to seek professional support from a mental health professional. When looking at the research, different studies, together with anecdotal evidence, there are various results in ratios between males and females identified as autistic, ranging from 2:1 to 16:1, respectively! So why are there such differences across studies? There are several possible reasons for this, some of them being:
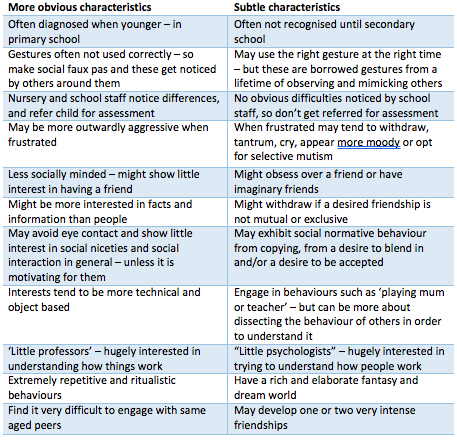
The below table illustrates the differences between more obvious characteristics of Autism compared to more subtle characteristics (National Autistic Society): Often, I hear parents say that their daughter’s teachers don’t notice any ‘problem’ in the classroom, and in fact, they’re considered the perfect student! This is often quite distressing for parents as their child may to experience intense emotional outbursts the moment they arrive home. Girls tend to mask their behaviours quite well, as they are more motivated to engage socially. They spend excessive amounts of energy doing so at school, as to not get noticed and fly under the radar. Because of this mental and emotional exhaustion, here comes the meltdowns when they finally feel like they can be ‘themselves’. The expressive language used by autistic females is often exceptionally good, which can then mask their difficulties processing verbal information. Their eye contact might also be quite good, they may do ‘small talk’ well and can be very chatty, though these tend to be quite exhausting and when their energy is not replenished, can cause significant distress and other mental health conditions over time. Females who seek therapy present with mental health issues such as eating disorders, personality disorders, depression, anxiety and self-harming behaviours that can divert the clinician’s attention away identifying these individuals as autistic. Mothers who identify with having autistic characteristics are typically the ones who bring their young daughters into therapy or for assessment, as they notice the difficulties in their child as similar to their own difficulties, and don’t want their child to go through the same challenges as they did growing up. Our mission at Hopscotch and Harmony is to smash the stigma of mental health conditions and a big part of our work is working with young children, teens and adults who are autistic. There is so much support out there and this will continue to grow as our understanding of autistic needs deepens. Listening to so many autistic individuals talk about their relief and enhancement of self-understanding when the assessment process identifies them as autistic are some of the benefits of going through the formal assessment process. Though this is not true for everyone. Some people identify with having autistic characteristics or self-diagnose as being autistic, and are content with being aware of their strength and struggles, and don’t want a formal assessment. Some people may overly-identify with a diagnosis and feel like ‘something is wrong with them’. This is where clinical judgement and parental intuition come into play… there is never a black and white answer, is there? Many psychologists at Hopscotch and Harmony are highly skilled in the autism assessment process. If you want more information on this process, please complete our assessment booking enquiry form FOUND HERE Being hated is not the goal in any relationship, and it can cut especially deep when the child you have loved and supported for years screams these words at you. Try these three approaches the next time your child shouts these words at you from across the room. Regulate Remember that feelings are catching. It is completely understandable that you are having a huge emotional reaction to hearing these words from your child. It will also only escalate the situation if you react from that emotional state. Make a rule of taking five minutes when you hear that phrase if possible to return to calm. Understand A child’s ability to feel and express emotions is the most developed part of their brain. That’s why they will often resort to exaggerated language in a highly emotional state. Try to approach this phrase with curiosity asking what is my child trying to communicate with those words? What big emotion motivates those big words. You will almost certainly determine that the emotion is not hatred but something closer to frustration, fear, or anger. Problem solve Once you and your child are both calm, validate their emotions by verbally describing what might be happening. ‘You said you hated me when I told you no more screens for today, I wonder if you are feeling a bit bored, and maybe even lonely?’ Again, a child’s strongest part of their brain is the region that produces emotions so sometimes they need an adult to model the rationale path out of a meltdown. “I hate maths!” might not be an unfamiliar phrase you hear from your child. But is there more to it? A Specific Learning Disorder in Mathematics (also commonly known as Dyscalculia) is a condition that affects a child's ability to understand and work with numbers. Here are some signs that your child may have dyscalculia:
1. Difficulty understanding and remembering basic math concepts such as counting, addition, subtraction, multiplication, and division. 2. Struggles with basic math facts such as memorizing multiplication tables or basic addition and subtraction facts. 3. Difficulty understanding and using mathematical symbols such as +, -, x, /, <, >. 4. Difficulty with spatial reasoning and understanding spatial relationships, such as left and right, up and down, or in and out. 5. Difficulty with understanding time, including telling time, and understanding the passage of time. 6. Difficulty with mental math and estimating numbers. 7. Struggles with word problems and understanding how to apply mathematical concepts to real-life situations. If you notice your child struggling with any of these areas, it's important to seek help from a qualified professional such as a psychologist, or a paediatrician who can refer you to the appropriate professional. Working memory is a process that allows us to hold and manipulate information temporarily in our mind in order to carry out complex mental tasks. Working memory is involved in many aspects of learning and development, as well as problem solving, and decision making. Working memory is limited in capacity and duration, meaning that it can only hold a certain amount of information for a brief period of time. This is why we often forget information we were just told, especially if we were not paying close attention to it. Children with strong working memory skills are better able to follow directions, remember information, and complete complex tasks.
Working memory difficulties can impact a child's academic performance and daily life. Children with working memory difficulties may have trouble remembering instructions, completing multi-step tasks, and paying attention in class. They may also struggle with reading comprehension, math skills, and problem-solving. It is important for parents, teachers, and other caregivers to be aware of the signs of working memory difficulties in children and to provide support as needed to help improve their working memory skills. Here are 5 ways you can help support a child who has working many difficulties:
As a parent, it can often be hard to support your child in moments when their only answer is ‘no’. This is where learning about developing a growth mindset can be influential in those moments and in supporting your child's development and success. Here are some things that can help parents to know when supporting their children about fixed and growth mindsets:
Overall, understanding and promoting a growth mindset in your child can help them develop the skills and mindset necessary for success in school and in life. At H&H we support children in developing a growth mindset in our individual sessions. We all know we need to prioritise our kids’ well being first after a separation or divorce, and that it’s important to work together with our ex to provide our kids with a stable and supportive environment, but that can also be really challenging at times. Here are some tips for co-parenting with an ex:
Communicate effectively: Effective communication is key to successful co-parenting. Keep communication respectful, focused on the children, and avoid discussing personal issues or engaging in any confrontational or argumentative behaviour. If things start getting tense, it’s best to walk away and find a different way to communicate - that might be through a shared parenting communication book, via email, or using a parenting app such as 2Houses or Our Family Wizard Create a parenting plan: Create a parenting plan that outlines custody arrangements, visitation schedules, and other important aspects of co-parenting. This can help you and your ex establish clear expectations and avoid conflicts. It can also be helpful if there is a custody dispute in court in order to demonstrate that you’ve both tried to communicate about these issues, and now need support via more official means. Be flexible: Be willing to be flexible and make adjustments to the parenting plan as needed. This can help you and your ex respond to changing circumstances and prioritise your children's needs. Support your children's relationship with your ex: Encourage your children to maintain a positive relationship with your ex and support their time together. This can help your children feel secure and loved by both parents. It’s so hard for kids when they want to talk to or about their other parent and they feel that they can’t do so without upsetting the parent they are with. Make sure that you let your kids know that you understand how important their relationship with their other parent is, and that they are welcome to speak to and about them at any time. Seek support: Seek support from a psychologist, support group, and/or your family and friends to help you cope with the stress and challenges of co-parenting. This can also help you develop strategies for managing your own emotions and supporting your children. Remember, co-parenting with an ex requires patience, understanding, and a willingness to work together. By communicating effectively, creating a parenting plan, being flexible, supporting your children's relationship with your ex, and seeking support, and keeping the focus on your children you can help ensure that your children are well-supported and cared for during the co-parenting process. Many of us have heard about mindfulness and it’s something we can all do in our day to day lives. Mindfulness is the practice of paying full attention to the present moment, whilst noticing your thoughts, feelings and bodily sensations without judgement. Mindful eating involves paying attention to the present moment and being fully aware of what you're eating, why you're eating it, and how it affects your body and mind. It encourages us to tune into our bodies and senses, and to approach eating with a non-judgmental, curious attitude. We often find ourselves gobbling down food whilst we’re sending important e-mails or getting the kids ready for school. Or we’re just so hungry, we inhale our food and find ourselves over-full and lethargic. Mindful eating can involve slowing down your eating pace, savouring each bite, and really noticing the textures, flavours, and smells of your food. It also involves being aware of your hunger and fullness cues, and stopping when you're satisfied rather than when your plate is empty. There are lots of benefits to your mental and physical wellbeing when you practice mindful eating. It can help you develop a healthier relationship with food, reduce overeating and improve digestion. It can also promote greater enjoyment and satisfaction with food, and act as a daily mindfulness exercise to connect to the present moment and reduce anxiety. Mindful eating is a valuable practice that can help us cultivate a more positive and nourishing relationship with food and our bodies, as well as using it as a valuable part of our day to be fully present. Next time you sit down to have a meal, take a moment to pause, breathe, and really appreciate every mouthful.
Dyslexia is referred to as a Specific Learning Disorder with an impairment in reading in the DSM-5-TR.
It is recommended families look for a specialised literacy tuition program that is designed for dyslexic children. These programs should have trained professionals who understand the needs of dyslexic children and can tailor their teaching methods to meet those needs. Check for the qualifications and experience of the tutors. Make sure that they have experience working with dyslexic children and have the necessary training and certification to provide effective literacy tuition. Look for programs that offer multisensory teaching methods. Dyslexic children often learn better through hands-on activities, visual aids, and other interactive methods that engage multiple senses. Consider the location, schedule, and cost of the program. Choose a program that is convenient and affordable for your family. Remember, what works for one child may not work for another. It may take some trial and error to find the right literacy tuition program for your child. Evidence-based programs and support for dyslexia:
Obsessive-compulsive disorder (OCD) is a mental health disorder that affects millions of people around the world. It is a condition that is often misunderstood, with many people not fully understanding the severity of the disorder or the debilitating impact it can have on a person's life. In this blog post, we will explore what OCD is and what it is not, and discuss how it can be effectively treated in a psychological practice setting. What is OCD? OCD is a disorder characterised by persistent, intrusive, and distressing thoughts or images (obsessions) that lead to repetitive behaviours or mental acts (compulsions) aimed at reducing anxiety or preventing harm. The compulsions may include physical rituals or mental processes such as counting, checking, or cleaning. These behaviours can become so time-consuming and distressing that they can interfere with a person's daily life, relationships, and work. It is important to note that having obsessive thoughts or engaging in compulsive behaviour does not necessarily mean that a person has OCD. It is only considered OCD when these thoughts and behaviors are severe, persistent, and interfere with daily life. Additionally, OCD is a distinct mental health disorder that is different from other anxiety disorders, such as generalized anxiety disorder or social anxiety disorder. What isn't OCD? It is important to recognise that not all repetitive behaviours or obsessive thoughts are indicative of OCD. For instance, some people may have habits or routines that they enjoy or feel comfortable with, such as arranging objects in a particular way or double-checking a door lock. These behaviours do not necessarily indicate the presence of OCD. Similarly, it is not uncommon for people to experience occasional intrusive thoughts or worries. However, these occasional thoughts do not rise to the level of obsessions that are characteristic of OCD. Effective Treatment for OCD OCD is a treatable disorder, and Hopscotch and Harmony Psychology offers several effective treatments that can help manage the symptoms. Cognitive-behavioral therapy (CBT) is one such treatment that has been shown to be particularly effective in treating OCD. This type of therapy involves identifying and changing negative thought patterns that contribute to obsessions and compulsions. Conclusion OCD is a mental health disorder that can have a significant impact on a person's life. However, with the right treatment, individuals with OCD can manage their symptoms and live fulfilling lives. If you suspect that you or someone you know may have OCD, it is essential to seek the help of a psychologist or other mental health professional. They can help identify the underlying causes of the disorder and develop a treatment plan that is tailored to your unique needs.
Are you the parent of a pre-teen and are unsure of how to approach the often awkward or uncomfortable conversation about puberty? It is great to feel prepared and informed about going into this conversation so you and your pre-teen can feel safe and supported to learn and grow together.
Puberty can have significant effects on the emotions of teenagers and pre-teens. During puberty, the body undergoes many physical and hormonal changes, which can affect the way they feel and behave. Here are some ways that puberty can impact emotions in teens:
Here are some steps you can take to talk to your child about puberty:
It's important for parents, caregivers, and educators to understand these emotional changes and provide support and guidance for teenagers during this time. Encouraging open communication, without judgment and providing a safe and supportive environment will foster your child’s wellbeing. Seeking professional help when needed can be helpful for pre-teens and teenagers during puberty as it can be difficult for them to speak to close family members about this often awkward topic. Parents and caregivers are valuable during this time as they can model healthy emotional expression and coping skills such as stating their emotions and engaging in self care. When parents/caregivers take care of their own mental wellbeing, they can better support their pre-teens. Everyone goes through puberty and emotional changes are expected and we all know it can be a tricky time, however these steps can help your child feel safe and supported. Being a parent can be one of the most rewarding experiences in life, but at times it can be incredibly challenging. This is true, in part, because being a parent is a time of constant change and learning, and because our children are just so important to us. It’s important to remember that it’s ok to recognise the challenge and real discomfort that is part of the job, and that you deserve compassion. Self-compassion is the practice of noticing your own suffering, and offering yourself kindness. Often, kindness is something we readily offer to others (including our children) but not always to ourselves. Self-compassion can help you manage stress, improve relationships and wellbeing. In this blog post we’ll explore the importance of self-compassion for parents, including some tips for practicing self-compassion in your everyday life. Practice is the key word here. Why practicing self-compassion can be useful for parents: Because you deserve it. Parenting can leave you feeling stressed. It’s common to experience feelings of guilt and self-doubt, and left unacknowledged, this can take a toll on your wellbeing. When you ignore the self-compassion you deserve, you are more likely to be critical of yourself, feel more overwhelmed and may find you have less ‘bandwidth’ for others. On the other hand, by practicing self-compassion, you may find you are better able to manage stress and improve your interactions with others, including those moments of high stress, energy and emotion. Self-compassion can also be a useful way to model healthy behaviors to our children. When your children see you treating yourself with kindness, they can learn to do the same for themselves, providing them with coping and resilience skills for life. Tips for practicing self-compassion as a parent: 1. Notice and acknowledge your feelings. When we are so busy and under pressure, it can be easy to ignore the discomfort underneath. If you’re feeling overwhelmed you may take a moment to pause, notice and sit with the feeling. Let it be and let it go. Some people find it useful to send an intentional thought inward, with kindness, to acknowledge the moment, such as simply saying “ouch… this hurts”. With practice, naming the moment, with honesty, kindness and acceptance, can help reduce stress, and improve our reactions over time. 2. Know that you are not alone. If you are feeling exhaustion, stress, guilt or self-doubt, you are almost definitely experiencing something like the experience of most parents. Some people find it useful to send an intentional thought inward, with kindness, to acknowledge that they are not different, broken or alone, such as simply saying “It is not just me… I am not alone”. With practice, this simple, kind message, can reset our emotional, cognitive and neurobiological systems, encouraging us to self soothe, connect with others and reduce the impact of stress over time. 3. Send yourself a word of hope or an offering of peace just as you would offer kindness and hope to someone else that you care about. Some people find it useful to send a simple, intentional thought inward, with kindness, such as “may I have the peace that I need”. Overall, practicing self-compassion as a parent can be an empowering and effective way to manage stress, improve relationships and increase overall well-being. By acknowledging your needs and feelings with these three steps, and by treating yourself as you would treat a friend (or your child!), it is possible to build a strong foundation of self-compassion that will help you navigate the challenges of parenting, whilst acknowledging your own needs as well. Many of these tips are based on Mindfulness Based Self Compassion. For more information you may like to check the official website here: https://centerformsc.org/ Tim Walker
Psychologist A cognitive assessment is a type of evaluation that measures a person's thinking abilities and intellectual potential. It typically includes a battery of tests that assess different areas of cognitive functioning, such as attention, working memory, processing speed, language, and problem-solving. As part of the assessment your clinician will undertake a parent interview to gather information about the child’s developmental trajectory and identify any factors that may have influenced their development. Cognitive assessments can be useful for identifying a child's strengths and weaknesses, as well as for identifying any learning difficulties or intellectual developmental delays. This information can help educators and parents better understand the child's learning style and needs, and can guide the development of individualised educational plans. Cognitive assessments can also help identify giftedness or advanced abilities in specific areas, which can guide the development of advanced or accelerated educational opportunities for the child. In addition, cognitive assessments can be used to monitor a child's progress over time, and can provide insight into the effectiveness of interventions or accommodations that are put in place to support the child's learning. Overall, a cognitive assessment can provide valuable information that can help parents and educators better understand a child's learning profile and tailor educational strategies to best meet their needs. Areas of cognitive functioning: Verbal Comprehension: Measures the ability to understand and use language, including vocabulary, grammar, and comprehension. Perceptual Reasoning: Measures the ability to solve visual problems and spatial reasoning, including the ability to recognise patterns and solve visual puzzles. Working Memory: Measures the ability to hold and manipulate information in the mind, such as remembering a series of numbers or letters. Processing Speed: Measures how quickly a person can process information and respond to it. Fluid Reasoning: Measures the ability to reason and solve problems using abstract concepts and logic. When speaking to the parent of an Autistic child, it's important to be mindful and respectful of their experiences and feelings. Here are some things you should never say to the parent of an Autistic child:
Instead, focus on offering your support and understanding. Ask the parent how you can help or what they need, and listen without judgement. Let them know that you are there for them and that you care about their child. By showing empathy and understanding, you can help create a warm and supportive environment for the parent and their Autistic child.
Exam periods can be a stressful time for students and their families. A certain amount of stress can work as motivation to study and focus on exam preparation, however large amounts of stress can be detrimental and lead to anxiety symptoms and avoidance behaviours. It can be difficult to know how to manage this balance.
Signs that stress has become unhelpful can include:
Exam stress can occur because of fear of failure, feeling unprepared, or perceived pressure and expectations. The good news is that you can do a number of things to reduce this stress. 1. Plan and organise your study schedule in advance. As soon as you know when your exams are put together a schedule:
2. Take regular breaks and engage in activities that help you relax. Build breaks into your schedule. Studying is tiring and it is important to give your brain opportunities to rest and recharge. Chose activities that you know give you energy, relax you or refresh you and schedule these into your study schedule. These activities could be medication, yoga, walking, playing games, reading, dancing … choose what works for you. If you find it hard to come back to study after a break, set a timer to go off at the end of your break or tell someone when your break should be over so that they can help remind you to return to studying. 3. Understand what environment you study best in and limit distractions. Ensure you have a space to study that is free from distractions. This might mean putting your phone on silent, face down and out of reach, or giving your phone to someone else during your study sessions. You might find that you study best at your desk by yourself with the door shut, or at the dining table around other people (or on a video call with a friend who is also studying), or in the school library with a group of friends. You might study best with headphones on or in complete silence. Ensure that your study space is clear and without distractions. If you do find yourself getting distracted, keep a notebook next to you to jot down distracting thoughts, and then deal with them in your break. 4. Make sure you eat and sleep well. It can be tempting to try to study every minute of the day, but it is important for your brain to get enough sleep and food. Ensure you factor sleep and three meals a day into your study schedule. 5. Talk to your family and friends about how they can best support you. Do you need your parents to help you keep you accountable? Perhaps checking in with them at the end of the day to see what you achieved. Or does having your parents ask about your study make you more anxious? Would you like your parents to help you develop a study schedule? Would it help to have a friend on a video call while you do homework at home, while they also do homework? Or would you just end up chatting? 6. Get creative with how you study. Try using study aids such as flashcards, mind maps, or practice tests to help you prepare. 7. Don't compare your progress with others. We are all different and this includes study methods and capacity. What works for your friend may not work for you. Try not to think of yourself as in competition with your classmates, rather focus on doing the best you can. 8. Use relaxation and mindfulness techniques. If you do notice your stress increasing, try closing your eyes and taking some slow deep breaths into your tummy. On each out breath, see if you can lengthen the breath and release any tension you notice. Our breath regulates our body’s stress response and slowing our breath can effectively bring our stress levels down. 9. Reward yourself. You’ve worked hard! After you have completed an exam or achieved an academic goal, reward yourself with something that makes you feel good. |
Categories
All
|
Hopscotch & HarmonyAt Hopscotch & Harmony Psychology, you can expect compassionate care and evidence-based guidance on your journey to wellness.
With clinics in Werribee and Belmont, as well as providing online counselling to clients who live throughout Australia, our dedicated team of psychologists and dietitians are committed to providing support to children, teenagers and adults. With a focus on understanding your unique needs, we offer tailored solutions to foster growth and resilience. Trust in our experience and dedication as we work together towards your well-being. Welcome to a place where healing begins and possibilities abound. |
Our services |
Contact usHopscotch & Harmony
Child, Teen and Adult Psychology Our Locations:
WERRIBEE: 1/167-179 Shaws Rd
BELMONT: 92 Roslyn Rd AUSTRALIA-WIDE: Online counselling |
Hopscotch and Harmony respectfully recognise the Aboriginal and Torres Strait Islander people as the first Peoples of the continent now called Australia.
We acknowledge the Bunurong and Wadawurrung people of the Kulin Nation, the traditional owners of the land on which we work, and pay our respects to their Elders, past, present and emerging.
© 2024 Hopscotch and Harmony Pty Ltd

























 RSS Feed
RSS Feed
